| 0:33 | Intro. [Recording date: January 24, 2020.] Russ Roberts: Today is January 24, 2020 and my guest is physician, author, oncologist, and Renaissance woman Azra Raza. She's Professor of Medicine and Director of the MDS center at Columbia University in New York. Her book is the highly acclaimed The First Cell. Azra, welcome to EconTalk. Azra Raza: Thank you so much, Russ. |
| 0:54 | Russ Roberts: Now, this book is not what I expected. It's a moving and inspiring mix of the personal side of being an oncologist, along with the policy issues surrounding the way we fund and do cancer research. It is a book about death and despair. It's also a book about hope and life. It's beautifully written. It's a powerful look at what it's like to have cancer, to work with cancer patients, and probably more than anything else a book about being a human being and all that that entails. I found it to be a hard book to read, and a hard book to put down. And, along the way there's a lot of policy about how we currently do cancer research. So we're going to, I hope, get into both sides of that--your personal story as a practicing physician and then also the policy issues surrounding cancer research. Let's start with just MDS [Myelodysplastic Syndromes], which is your specialty. What is it? And what's its relationship to leukemia and cancer generally? Azra Raza: That's a good place to begin Russ, because my career started with this. In fact when I came to the United States in 1977 as a fresh medical graduate I was hellbent on studying and treating acute myeloid leukemia, a liquid cancer which is easier to study than a solid tumor like lung cancer, ovarian cancer, etc. By 1984 it had become very clear to me that in my lifetime we will not be able to find the solution for acute myeloid leukemia, because it is a ghastly disease and tremendously complicated. But, then, many of the patients would give a history of having had a pre-leukemic phase in which their blood counts were falling, they were developing anemia, their white count was going down. And, these syndromes were eventually gathered under the umbrella of myelodysplastic syndromes, or MDS, which is really a disease by itself that can kill, but a third of these patients can develop acute myeloid leukemia and die. So, I turned my attention towards catching patients' disease, or acute myeloid leukemia, early by trying to catch them at the MDS stage. So, I was really interested in the pre-leukemia part of this MDS, to begin with. |
| 3:25 | Russ Roberts: Now, you summarize our current approach to cancer as a 'slash, poison, and burn.' What do you mean by that? What does each of those mean? Azra Raza: Slash means surgery. Poison means chemotherapy. And burn means radiation therapy. Russ Roberts: And what would you say is the mix of those three in our current--that's our arsenal of weapons. Has that arsenal shifted over time? Or has it changed much? Or are we still doing a lot of each? Azra Raza: This is one of the main reasons for me to become an author suddenly, because I'm not a writer. I really am an oncologist and a scientist and I've dedicated my whole life to treating patients and trying to study their disease in the laboratory. But, I was forced to take the pen on, because--while it is very true that we are killing 68% of cancers we see today, the reason we are curing them is mostly because of early detection. And, the treatments we are giving them are, by and large, the same treatments that we have been giving for 50 years--which is the slash, poison, burn. Now, many of my oncology colleagues tend to have this attitude towards me saying, 'Azra, we are looking at the glass being half full and you're looking at it being half empty.' Which means, 'Why am I asking even the question that 68% percent of patients aren't being cured?' We should be pumping our chests. We should be giving ourselves gold medals. We should be proclaiming this from the rooftops-- that we are curing almost 70% of cancers diagnosed today. But, I think that would be unfair to patients coming in the future. One of our family friends once told my younger brother [inaudible 00:05:47] that, 'Look if the sun rose from the West, everyone will stop and stare at it and wonder why. But, there are a few people who see the sun rise in the East every day and wonder why.' In other words, there are people who refuse to take things for granted. So, I am questioning, Number One, why is it that we are continuing to use the same old, same old, same old treatments despite billions of dollars being invested in trying to develop new, targeted, non-toxic, non-chemotherapeutic therapies? Why are we not looking to determine the reasons for 95% of clinical trials failing in cancer today? What pre-clinical platforms are we using to bring those drugs to market? And, then on the other hand, the 30% person of patients we are not curing because they were diagnosed at an advanced stage of their disease, their outcome today roughly is the same as it was 50 years ago. Even with this slash, poison, burn, we have made no difference to them. So, basically what is the glass half-empty and what is the glass half-full here? You are using the same treatment. We are benefiting the patients we would have cured only because of earlier detection. And, the 30% are dying terrible deaths. |
| 7:28 | Russ Roberts: Yeah; I would say your book is a shout from the rooftops that 68% is not enough. And, I think the other point, which your book painfully makes clear, is that for those 30%, the slash, poison, burn is--it's a cruel approach, unbearable approach for a doctor who has pledged to first do no harm. We should probably explain. People who have had experience with cancer or loved ones with cancer understand this, but you should explain why you use the word 'poison.' The technique of chemotherapy, which is the poison part of your trio, why do you call it poison? What is its modus operandi? How does it work? Azra Raza: It's literally, somebody described it taking a baseball bat and hitting a dog with it to get rid of its fleas. That's what giving chemotherapy is. Chemotherapy cannot distinguish between a normal cell and a cancer cell. But, it kills rapidly-dividing cells. That's why side effects of chemotherapy affect rapidly-dividing normal cells the most. For example, hair fall-out, because hair follicles grow very fast. Or we have severe nausea and vomiting because GI [gastro-intestinal] tract is sloughing cells and diving very rapidly. So, chemotherapy basically is a sledge hammer that goes in and starts killing cells, and because cancer cells are dividing faster than normal cells in an organ, we kill more of the cancer cells and less of the normal cells. But, still normal cells die. And, by the way Russ, let me stop here and tell you one other thing. We are talking a lot about immune therapies these days, and there are multiple kinds of immune therapies. But, the most dramatic ones are those that use bodies' own immune cells to activate them and attack the cancer. You might have heard of CAR-Ts [Chimeric Antigen Receptor Therapy]. Nowhere do investigators point out that while CAR-T cellular therapies, the most dramatically effective form of killing every last cancer cell in the body. I acknowledge all of that. It is a fabulous feat of scientific achievement. Russ Roberts: Incredible. Azra Raza: Incredible achievement to take the body's own T-cells, which are a kind of immune cells, and engineer them in such a way that they are now carrying part of a B-cell, which is another lymphoid immune cell. And it's activated to kill any cell it means that is expressing a B-cell receptor, CD-19. This is the most common CAR-T therapy used for B-cell lymphoma or leukemia. But, nowhere do investigators point out that these T-Cells also cannot differentiate between a normal cell and a cancer cell. So, what they actually do is kill the whole organ. But specifically that organ. Still there are off-target effects, which means other cells in the brain or somewhere else which are expressing the same marker. These engineered cells are so effective they will seek out and kill every cell that even has a molecule of that receptor being expressed. |
| 11:21 | Russ Roberts: So, I saw the movie Breakthrough, which I recommend to listeners. It's a documentary about Jim Allison, who was a pioneer in these techniques. And it's a very interesting movie for a bunch of reasons, and I think some of them will come up through the course of our conversation. But, the one I want to focus on is, it's a very celebratory movie. It is yelling from the rooftops that we've made an enormous amount of progress and it highlights some wonderful, miraculous, heartwarming stories of people who had a death sentence that was revoked, and they're fine. It's not just like they're alive. They're doing well. And, what the movie leaves out--as the economist I had to notice the two things, the most important things, it leaves out. One is: it doesn't help that many people. It's a very small group: unfortunately it's a small group that these techniques are working on with that kind of effectiveness. Second thing, they don't talk about the cost. In fact, the pharmaceutical company in the film, the courageous one that keeps the trial going that was a failure--there's some great wonderful things there. But of course, they have to compensate for their enormous risk they take in extending a trial way beyond its normal time, which of course could have failed and cost them 100s of millions of dollars. It turned out it worked. Which is great. But, anyway, cost is ignored, which it often is in these kinds of stories. And, then it ignores the fact that it's a small group. And that's the tragedy that you're focusing on. The breakthroughs that we have made have been, as you say, some of them have been just glorious. But, unfortunately, they don't apply very widely, at least yet. So, react to that, and also the possibility that it might expand to treat other cancers that we don't know about right now. There might be other forms of this therapy that could reach a wider range of people. Or is that not the case? Azra Raza: Russ, one of the big problems we have faced in cancer is that, despite looking for 60 years, we have not been able to find molecules that are expressed only by cancer cells and not by normal cells. In other words, we can't find the address, the unique zip code, of a cancer cell so far. So, at best what we are trying to do is basically kill cells more effectively irrespective of whether their cancers are normal. When you ask me that, 'Will this immune therapy be applicable to other cancers?' Absolutely. It should be applicable. But, right now it is not so because if we try to kill liver cancer cells with this kind of CAR-T therapy it will destroy the whole liver, not just liver cancer cells. Or, it will destroy the whole GI [Gastro-Intestinal] tract, the whole colon. So, the entire organ would be killed because normal cells are expressing the same markers as the cancer cells. However, when we learn to identify by means of whatever biomarkers we develop, in the future as technology is evolving, then not only would we be able to specifically target cancer cells, but the other thing is that we would be able to use these therapies in earlier stages. So, that right now, when we give these therapies, the only patients who respond are the ones who experience the most severe side effects, called the cytokine storm, which basically puts the patient's life at stake. That, if they survive it, they will enter remission. Those patients who don't experience this horrendous cytokine storm, they don't even eventually respond to this kind of therapy. In other words, what I am saying is that we are going in the right direction. We have made some significant, dramatic advances in these kinds of immune therapies, but the way they are talked about, the hyperbolic language that is used minimizing not just the financial toxicity but actual physical toxicity of immune therapies. And, then let's take just chemotherapy. You asked me why do I call it as this poison? It's because recently I saw a 42 year old beautiful woman who came to see me because suddenly she had developed weakness and fatigue and was seen by her primary care physician and found to have low blood counts. I do a bone marrow and find that she has acute myeloid leukemia. Now, I look at this gorgeous young woman, who's toned and tanned and I shuddered to think what I will be doing to her, what she will look like in another six weeks after the chemotherapy we give her. So, the question I'm asking is, I was giving the same two drugs in 1977 to treat a patient like her that I'm using today in 2020. The same two drugs with the same dreadful results. How long will we continue to do it? What is there for the future? How can we change it? And, one of the worst things, and the last thing I want to say about it is: Do you know to this day we don't know how those two drugs work? We have no mechanism of action precisely laid out for them. So, what is that, once we have made an acute myeloid leukemia then? |
| 17:22 | Russ Roberts: So, part of your book is an indictment of the--I don't know what you want to call it--the intellectual infrastructure of the pharmaceutical industry and the research behind it, both private and public, that uses a set of clinical trials--typically on mice and then it goes up to a larger animal, typically I think a dog--before it goes to a human. And, we understand that it's hard to experiment on humans for lots of reasons, but your point about mice is that it's not just, 'Well, you know, not every time it works out that it works on a mouse, it doesn't work on a human.' In fact, it almost never works on a human if it works on a mouse. And, this whole intellectual structure is a mistake, in your view. It's a reductionist attempt to hone in on the micro-cellular level for this causal, 'You know, we're trying to close the door on this one little entry,' when in fact that whole approach, you're suggesting, is wrong because cancer is so complex. And, it's not just complex meaning it's hard to figure out. It's complex meaning it's multi-variate, and it's different in every person, even. And, so the whole approach we're using of this mouse-driven, reductionist approach at the cellular level has failed, more or less, and is unlikely to get any better. And we're throwing hundreds of billions of dollars at it. Azra Raza: You said it better than I could have said, really. Russ Roberts: Well, I read your book. Azra Raza: Well, I'm glad I have a convert. Russ Roberts: Yeah, well, I'm worried about it. Well, go ahead. Azra Raza: No, I was going to say that science has succeeded where magic failed because we are interested in understanding things; and we think that we learn to control nature, and that power will be the byproduct of our understanding. And, that is why I think the intent to try and study and understand cancer has got to be applauded. The problem is there aren't that many cancer cells available coming from humans for basic scientists to study, so they have gone ahead and made models. And, again the intent is very good, and to study the biology of cancer, animal models are fantastic. So, I want to make this distinction very clear, over and over: that I'm not against the use of animal models and mouse models to try and understand the mechanisms, the biological basis for phenomena that we observe. That's all exactly what these models should be used for. But, there seems to be an emotional Mason-Dixon line cleaving oncologists from basic scientists when it comes to developing new chemotherapies. My contention, Russ, is that all research on cancer should have one, and only one, goal, which is to benefit the cancer patient. It's all very well to study biology in mice and rabbits and fruit fly and zebra fish. But, if it is not therapy-driven, if it's not going to help my patient, then for me it is of no use. And, spending hundreds of billions of dollars to identify the next intracellular signaling pathway in a tumor that is artificially created in a mouse is complete waste of money for me. Especially when we talk about drug development--the idea that we can create a tumor in an animal model, treat it with a given agent and then bring those results to the human bedside. Well, this is met with unmitigated disaster. And the reason that you have very clearly pointed out is, yes cancer begins in one cell, but the cell keeps dividing. It's covering one generation within hours, which it should normally cover in months, if not even longer. So, that these rapidly diving cells made DNA [deoxyribonucleic acid] copying errors, which are known as mutations, every time a cancer cell divides into two, it picks up new mutations, which means now there are potentially two entirely new cancers. It's something like the brain has 100 billion cells, but one quadrillion connections. The same way a cancer begins in a cell but then it has the potential of constantly moving, constantly changing and undergoing metamorphosis so that within days there is now a mixture of heterogeneously, biologically distinct populations of cells within in a tumor. And, I always say that treating cancer like one disease is like treating Africa like one country. It's not the same even in two sites in the same patient, or two days in the patient. The tumor has changed. So, how can we apply a reductionist approach in this tsunami of chaos within a tumor, along with its micro-environment, the intracellular signaling, the immune response, the blood supply, the angiogenesis, taking all of this complexity and trying to bring a reductionist scissors to it and trying to find one molecule and develop one magic bullet for it, it hasn't worked for 50 years. This is why--Sorry. Russ Roberts: No, go ahead. Finish your thought. Azra Raza: I was saying this is why 50 years later we are still using slash, poison, and burn, and the other 30% patients are still dying the same way, and for the 70% we are using slash, poison, burn, we don't even understand how those things are working. Russ Roberts: Azra, I was just going to say, I think you were wrong--you said I said it better than you; but I think that was not true. That was beautifully said. The other part of this, of course, and we've talked about this on other episodes related to these issues. And, let me try to summarize this--this is the way I see it as an economist. We have a Medicare system, which is for old people, which does not negotiate drug prices, and as a free market economist I love that we don't negotiate our price. I don't think the government should be setting the price of drugs. I don't think that's a good thing. However, at the same time--and these two things don't work well together--at the same time, any increase in efficacy, no matter how tiny--an increase in life span, a median increase of two months--now becomes the gold standard of treatment and is paid for by Medicare. So, basically there's an enormous incentive, which the drug companies have--pharmaceutical industry--to make marginal improvements at enormous costs, creating new drugs that can be patented, which they of course have an incentive to find, that are paid for by a third party--me, the taxpayer--without regard to whether that money is worth it. There's no skin in the game. Or I would say it differently: it's the wrong skin in the game, for the pharmaceutical company. They are motivated by profit, which is a glorious thing. You say so in the book at one point in a sentence I'm not going to quote but it's really well said. Basically you say: you give people a goal and an incentive to find it, they'll work at it. And, yet we've created a set of incentives for the pharmaceutical industry that is not healthy. And that combination of patent protection, marginal--and I mean marginal meaning small--increases in efficacy, paid for virtually without any restraints, is an enormous waste of money. And, your book, you're not an economist but much of your book could be summarized as saying the cost-benefit of this is out of whack. This is not an effective use. Now, that story you just told of why the current approach doesn't work well, you could react to that with despair. You could say, you certainly at a minimum don't want to throw good money after bad to continue that approach, which is what we're doing in your view. The question would also then be, what would replace it other than despair? If the current approach is an utter failure in your view--and I'm going to maybe push back on that in a minute, but let's start with that--if it's an utter failure and it's financially a mistake the way it's structured to waste resources relative to return, what might replace it? What could do better? Azra Raza: I think, again, excellent analysis of our healthcare doldrums right now. It's no surprise that only 20% of Americans have any confidence in the healthcare system today. In fact, 20% Americans are being hounded by collectors for medical bills. Russ Roberts: Yeah we had a recent episode on that. It hasn't aired yet, but with Marty Makary on this problem of unpaid bills. I would say, though, Azra to be fair, I think most Americans love their healthcare system. And, I think it's actually a quite high number. I think the recent polls I saw--I don't know if it's a good poll or not, have to be careful--but it's something in the 80s: 80% or more are satisfied with their healthcare. We have extraordinary healthcare in the United States, for most Americans. Not all. Many Americans have horrible access to it. Too many. But, so many have a gloriously, fabulously innovative and technologically advanced amazing set of options and they're delivered without waiting; and you get access to incredible minds like yours, and training and experience, and it's sometimes even done with compassion. So, it's a wonderful system but the price that we pay for it seems to be way out of whack for what we get in return. And that's simply--the reason I think we're so happy with it is we don't have to pay the price directly. We don't realize what the full price is. |
| 28:27 | Russ Roberts: But, I want to move away from, unless you want to add something, I want to move away from this issue of the overall system and just focus on what you think the best--your book is called The First Cell for a reason. What do you think we should be doing differently? We need a different approach. Azra Raza: Yes, thank you so much for bringing me back to the important--the optimistic part of my book. Although, Russ, I have to say that the subtitle of my book is almost as important as the title. The subtitle is The Human Cost of trying to continue to persist in the same old, same old, because this is why I look at everything we are doing in cancer through the prism of human anguish. What are the patients and their families going through when we practice the current form of treatment? Clearly if we treat a disease, any time we treat a disease, we have a 50% chance of winning and 50% chance of losing. But, the way I have tried to look at it in the book is if we treat the person, then we have 100% chance of winning. We have to stop the self-deception that is limiting our ability to risk new areas of research and give up the sclerotic old ones. One thing we learn in medicine over the years of practice, and seeing, as I do, 30 to 40 cancer patients every week for the last 40 years--one thing you learn is that: how you want things to be makes no difference at all. And, at every step of the way, I have to stop and ask myself, 'What is the categorical imperative at this point? What should I be doing for this patient that should become not a model--as categorical imperative?' And, this is what brings me to look at the whole cancer issue in a different light now. So far our strategy has been, as you and I have been discussing for the past 45 minutes, is that we try to kill every last cancer cell in the body. But, the only thing that's really worked for cancer in the last 50 years is that we have brought down cancer mortality by 1% a year. Which is no laughing matter, nothing to frown at, because that has translated in the last three decades into a 27% decline in mortality. But, most of that has happened for two reasons. One, because the anti-smoking campaign finally began to show some results, so that the kinds of cancer we were seeing associated with that have declined. But, more importantly, or equally importantly, is that we are detecting cancers earlier and earlier, instituting whatever terrible treatments we have, but at least instituting them early. So, we know clearly since 1907 that it's not cancer that can kill but it's the delaying the treatment that kills; and the earlier we detect the disease the better, and then we have to try and kill every last cell. Yes. But, we are not detecting cancer early, so the question is: Why in this day and age of supreme technological advances, magnificent scanning and imaging devices and handheld devices and cellular forms, etc., and self-driving cars--why are we still using 50-year-old methods to look at PSA [prostate specific antigen], to look at mammograms, or to put a tube into someone's gut to try and find a cancer by looking for it? Those really have to be changed. So, how do we change them? Russ Roberts: And before you do that, I want to say that when I first heard the title of your book and I read a brief a description of it, I thought, 'I'm going to hate this book.' Because, this idea that we need to screen more effectively, which is a big theme of the last 25 years--get your colonoscopy once you turn 50; get your mammogram once you turn 30, maybe even, or 40; get that PSA test--many of these screening techniques as we've talked about many times on the program, and as you talk about in the book, they've led to more harm than good. We're not going to talk about each one individually and we're not giving medical advice on the program, but I think listeners know well what some of these tests are and you should read about them before you just unthoughtfully just get one, because you hear that it's a good idea. Many of these tests, the false positives, the test itself, the anguish, the damage it's done is worse than the disease. The net effect is often zero or negative on mortality. And, so when I first heard about your book I thought, 'Well this is going to be an easy book to dislike because the idea that we should screen earlier and often,' and of course there are people such scans and say, 'You could have cancer right now. Go look.' And, my view has always been, most of the time it's better not to look, at least under current technology. So, I was relieved reading your book that you know all that, of course. So, when you talk about earlier detection and screening, you don't necessarily mean the current arsenal, which is I think a tragedy in many cases. I have Vinay Prasad coming on the program soon, and he's written very powerfully on Twitter and he's got a new book coming out which I'm going to read for our interview, called Malignant. Which, he's very aware of these failed screenings. So, when you advocate for the 'First Cell'--meaning the very beginning of cancer and nipping it in the bud--you're not saying we need to do more of the current set of screening. What do you have in mind? Azra Raza: So, what I have in mind is that we--I myself just talked about the failure of the reductionist approach that basic scientists and oncology researchers have used to try and look for one gene and try to find a magic bullet to undo the harm that gene is doing. But, in fact we are all guilty of this reductionist approach. So if you think about cancer, there are cancer cells; then the cells have DNA in the genes. DNA transcribes RNA [ribonucleic acid], and this is translated into proteins, and then proteins are metabolized. So, now we have five compartments--cells, RNA, DNA, proteins, metabolites. Why should we look at any one of them or any one gene in DNA or any one protein signature? We should be looking at everything simultaneously. So, with this kind of an approach, which is more pluralistic, using the latest technology, what I am proposing is that there are patients who have cancer today. Many times I am asked this question, Russ: 'If you have acute myeloid leukemia, Dr. Raza, you are being so critical about the treatments,' and they will say, 'Would you take the treatment?' My answer is, 'Of course I'll take the treatment, because every human wants to have hope. I want to be that one unicorn who's going to be the exception. And, 30% patients with acute myeloid leukemia will survive five years even today.' So, I'll take that chance. Sure. But, the question I'm asking is: Why is this the only choice being offered? How can we do better tomorrow? So, now it comes to two issues. One is that we have patients today for whom we need treatments and we need to invest resources to try and improve those treatments and find better ones. I'm saying that the other half of resources need to go to improve the technology we have for earlier detection, which means a really serious, thorough, overall analysis of cells, RNA, DNA, proteins, metabolites from serially, sequentially studied actual human samples, not animal models. And, the last thing I want to say about this is that this is where real and large-scale studies will have to evolve to provide the sample size for machine learning and artificial intelligence. Since 1984 when I turned my attention towards studying pre-leukemia and following these patients as they are either died of MDS or developed leukemia, I started banking bone marrow and blood samples of my patients. Today, Russ, this may sound like a very ordinary thing; but I have now collected over 60,000 samples from thousands of patients. Not one cell in my tissue bank has come from another investigator. All of these patients mean something to me because I've personally taken care of them. Most of them I have done with my own hands. This is a tissue repository where, today, I can go in, look at the cells, look at RNA, DNA, proteins, and metabolites in a serial fashion--as the patient progressed from pre-leukemia to acute leukemia. This is how we can work our way back and then ask the question, why did some patients get pre-leukemia? What were the risk factors that made this individual or these people susceptible to getting pre-leukemia, even? And, this will take us then to identify a group who is at high risk of developing pre-leukemia and then we can start monitoring those individuals, healthy individuals who are at high risk, in a targeted fashion. So, I can do this for pre-leukemia and acute myeloid leukemia. The resources are needed. I'm making this appeal to everybody that we should not rely on any one test done annually which was developed 50 years ago. Rather, we need to develop using the latest scanning, imaging, biomarking, genomic, proteomic, metabolomic technologies to find maybe 500 different tests that can be amassed in a bar code fashion or can be done rapidly, quickly, to identify individuals in the earliest stages of cancer. The resources, half the resources, go to treating current cancer patients and developing and improving treatments for them. The other half must be invested towards early detection through the latest technology and prevention and nipping the cancer in the bud. |
| 40:07 | Russ Roberts: So, the way I would think about it, and you talk about it in passing in a number of places in the book, is that: When you've used the word 'reductionist'--you're focusing in on a--you're not focusing in; you're talking about researchers who focus in on a small causative window that does not capture the full building. And you have an amazing story which I just want to read because I loved it so much. You were talking with George Washington University Dr. Ayub Ommaya, a neurosurgeon. And he was talking about the brain. And, you asked him, 'What would be the final level of reductionism needed to site the root of consciousness?' Meaning: Where are we going to find consciousness in the brain? Is it over here? Is it over there? Is it the amygdala? Is it the frontal cortex? Is it the [?] vivida? And, his answer is a deep insight that is very relevant for economics and life. He said the following, quote: "Azra, taking apart the Taj Mahal brick by brick to discover the source of its beauty will yield only rubble. It is the same with the brain. The emergent complexity from simple individual parts accounts for its essential mystery." And, you add: "It is also the reason why cancer will not yield its secrets through a reductionist approach." Of course, that reductionist approach is how people are trained. It's how people grow up in medical school. It's how they grow up in pharmaceutical research. It is the default. And by the nature of our scientific funding system where existing scientists approve grants to new scientists, typically, in the place of bureaucrats, it's sort of better. But it's got the problem of group-think. And, you are demanding--and it's beautiful--and you are demanding, not an end to that groupthink--because you concede, and I think you have to concede, that there have been advances through that. I was going to push back against you earlier and say, this animal model, if we hadn't followed it we wouldn't have gotten to it, we wouldn't have gotten to these these immune therapy techniques, and they have led to a lot of good things. Even if it's only 30%, it's 30%. Better than nothing. Whether it's worth it is a different question. Your point is that we need to try some different approaches. And the current system is not designed for imagination. It is not designed for creativity. I mentioned Jim Allison earlier, who was a key part of this in the documentary Breakthrough. It's pretty obvious when you watch that film that Jim Allison is not normal. Thank God. Jim Allison is a maverick. He was a crusader who was overconfident--could have been wrong--but believed in a set of observations and a strategy for fighting cancer that people had seen fail over and over and over again, this idea of immune therapy. And, it failed. It's not just like, 'Oh, he tried this and it worked.' It failed over and over again. Yet he persisted. He stood on that rooftop and said, 'I think this is going to make a difference,' and he did. And, I would argue that the current system needs a lot more trial and error. It's the wrong kind of trial and error we're using now. This reductionist, animal, mice-based approach. We need a world where there's a bunch of islands where people are trying radically different approaches that you're talking about. And, I know we have listeners to EconTalk who are capable of funding such approaches; and I know you know about some of those who aren't listeners. But it seems to me you need a very wealthy person who doesn't--who sees the world through your eyes and says, 'Enough. We need to stop spending as much money as we're currently spending on this, and the current system's not designed to change.' So, we need to have an end-around. So, that's why I see your book as a--I mean it's possible that the FDA and others, the National Cancer Institute, NIH [National Institutes of Health], will see that you're right. But, it's also, I think, more likely, and the history of science to me bears this out, that someone will say, 'Let's try something different. Let's try something radically different. Let's dream.' And, most of those dreams will fail. It's just the nature of things. But, as you point out, you have a wonderful data set, this tissue repository. You just need some money to help let it shed some light on things. Azra Raza: Not just some money. It needs quite a bit of money; and the money is very easy to raise, actually. Because one thing I would like to point out is that one in five new cancers occur--and, I don't want to scare anyone Russ, but statistics are important in some places, and unless we are aware of the tiger in the bush we are not going to be careful. So, this is why I point this out to you that one in five new cancers appear in a cancer survivor. And, the worst case was my husband. He had the first cancer at 34 years of age, and a completely different one at 57, of which he died. Because the underlying reasons that led to the first cancer are still there, and then we have also created more damage by giving chemotherapy for that first cancer. But, luckily we are successful in treating 70% of cancers, almost, today, so that there are a lot of cancer survivors. 2020: 16 to 17 million now; and by 2025 there will be 20 million cancer survivors. They are the ones who should be most carefully watched and monitored for the appearance of the first cell. If only one million of them give $10 a month for a year, that is all I would need to study the tissue repository. That's the kind of public awareness that could really help do this sort of thing. And, the other model is what you suggested that a great philanthropist with a big heart suddenly realizes that: yes, here is some tissue that has been collected for 35 years and it's sitting in freezers right now. Whereas, if we invest this money, within a few years we will have all of these multiple compartments well studied that I talked about. And, surely, even if we don't find the first cell within the next two years, we will have so many new insights into how this disease is progressing and expanding and killing that all of this would be worth our while. I don't think that it's very important for the public at large to understand that not--the kind of smoke and mirror we have used to convey cancer news seems to have created an impression in the public that great advances have been made. Unfortunately, I don't agree that great advances have been made, while fully admitting--and, there's no reason to deny: I am very much on the front lines myself, Russ. So, there's no question that I'm doing this every day. It's not like I'm some author who is writing this research. I am seeing 40 patients a week. I am a cancer widow. And, I am in a lab doing basic research for 35 years, so I don't need to be lectured by anybody about how much advances have occurred in cancer. Of course I appreciate them. I practice them. I told you I would take the same treatment that's offered if I get acute leukemia today. My husband took the treatment. I gave it to him. The same treatment that killed his entire immune system and eventually caused such severe infection that he died of sepsis, but I gave it to him because it gave him a chance of survival also. And, he did survive for five years thanks to the treatment we gave. Russ Roberts: That's a tough five years. Azra Raza: Yeah, it was very tough. And the point I make now is that it's just unfair to patients coming in the future to keep insisting that we are making great advances and this incremental success is fine and we should keep investing $150 billion dollars a year to treating cancer and whatever number we spend in doing research in the same old, same old way. No, I do think that we can see clearly what is failing and instead of investing--I'll give you one last example. Let's say that this immune therapy is working in lung cancer. And, one drug-- Russ Roberts: Seems to be doing some. Azra Raza: Yeah. Let's say it gets approved: immune therapy gets approved. The same immune therapy has also worked in, let's say, a melanoma. Now they do a trial in multiple myeloma and other bone marrow cancer, and what happens is that instead one trial there are not 500 trials, there are not 1000, there are 2200 trials going on to ask the same question. Now, each clinical trial costs millions of dollars. Phase One costs $25 million, and Phase Three costs anywhere from $500 million to $2.5 billion dollars. Why do we need 2200 trials to ask the same question? Instead of all this redundant waste of resources in trying to make a quick buck, through which we are stifling creativity--we are stifling research and development of normal[?novel?] targets because we are just trying to rush and make money by, 'Me too, me too' kind of approach. I'm insisting that we stop all of that and redirect the resources. There's plenty of money. For God's sake, America's the most affluent country in the most affluent of times. We should be able to invest in this properly and really make sure that the future cancer patients are served better. Russ Roberts: Well, I want to come back to emergence. I think one of the challenges here is that you may see that as wasteful; the current incentives encourage it. Some good things come out of it, but for all of its flaws, it might be better than a Cancer Czar who allocates money, unless you were the Czar. If you were the Czar, you might start acting differently once you became the Czar. And, czars tend to stifle creativity, generally, as well. So, it strikes me, when I think of the institutional changes that I would think about to get us closer to your vision than the current one, a set of prizes would maybe be a better idea. There are a set of prizes, of course, built into the system right now. Just that those prizes are structured in ways that encourage another slice of the salami rather than a different approach that might have a much bigger impact. So, I think it's a very tough problem, and I think politically very hard to change that current system. And, your book is an attempt to raise consciousness about it. I think that's great. Listeners to this program maybe will nowt think a little bit differently about it, but it's a hard problem and I think the end-around approach is ultimately probably where we need to get to. We see this already in the way technology is being used for medicine in creative ways outside of the current system, whether those current system will approve those ways for funding, etc., of course remains to be seen. |
| 52:25 | Russ Roberts: Let's switch, if we might, to the personal side of the book, which was really devastating and inspiring at the same time. You have a lot of stories about the suffering of patients, and when I first started reading those parts of the book I actually thought, 'Why is this in here? It's depressing. It's sad, a 23-year old dying of cancer surrounded by friends and parents. It's unbearably sad.' But, there's two things about it that I think are important. One is it's beautifully written. It's inspiring the way people can love in those settings. But, more than that, it reminds you--and you have to remind people--of what's going on behind closed doors in the halls of the buildings that you're in every day and that the rest of us mercifully are not. Which is that human toll, and it is very, very difficult and very powerful. So, I want to talk a little bit about that personal side. You mention the death of your husband--you write about in the book. You talk about in the aftermath of that you were, I would describe it, you were in a daze. And, you talked about fiction and reading helped you. Tell us about that. Azra Raza: Yeah. You're so right about this, Russ, that the science can finish but the human stories go on, and I do think that the most important part of my book relates to the patients who are living today who agreed to write in the book their own wonderful experiences through terrible times that are the only beacons of hope in this terrifying darkness that cancer brings with it. And, the fact that families of these patients were willing to be interviewed and when I asked them to cast a backwards glance on their experience and see what parts they could have changed, what decisions they could have altered, now with the luxury of time and with the acceptance that comes eventually with time, what can they point to that they should have done differently? And I think that those are the most powerful and moving statements coming from the families when they talk about their loved ones dying. It's true that the dizzying and disorienting daily challenges of cancer can really bring a fog down upon you, a daze upon you. And, no sooner do you get used to one situation that suddenly everything changes and now you have to adapt to completely new findings and new test results and new challenges and new physical symptoms, etc. It's very difficult. So, an important part of the book is looking back, trying to bring some method to the madness and eventually coming to the conclusion that, in fact, the only answer is that there is no answer. That we are trying to bring some sort of rationality to randomness and disease and none of it makes sense. And, at some level, one needs to accept it. How do you develop this ability to continuously witness the kind of pain and suffering and anguish that people are going through? At one point, for me, poetry has been very important, Russ. Because I come from an intensely and a deeply oral culture where reciting poetry and memorizing poetry is CRISPR'd [clustered regularly interspaced short palindromic repeats] into our DNA at birth. And, growing up at home in Karachi, Pakistan, my parents made it a point that all seven of their children were made to memorize hundreds and hundreds of verses in Urdu and English, and sometimes in Persian as well. And, very often the kind of two lines of a ghazal, which is a form of a very stylized poetry in my language, Urdu--two lines of this form of poem are to me like two strands of the DNA. In a microcosm is contained the macrocosm of meaning. And, it teaches you things that are impossible to verbalize, often. And, at one point, I remember when I was 32 years old and faced with one of my patients, J.C., who was extremely ill, and she was only 34, so we were practically the same age. And, one day instead of telling her jokes, trying to distract her, I read her a piece of a poem that I had memorized, which I'll recite for you just now and for your listeners. It's a poem by Subhash Mukhopadhyay, who's a Bengali poet, and it's a translation. This condition of life is not for the whole year.
Only for the few months when it rains,
the blazing fire of the dry wood will cook rice in no time,
and whatever is there will come back into view sharp and clear.
When the rains depart, we will put out in the sun everything that is wet, wood chips and all,
put out in the sun we shall, even our hearts. And, reading this poem to J.C., we both just burst out crying at the end, and it was some form of a catharsis for both of us. And, J.C. was someone who is dying at 34 who has two-and-a-half year old twin daughters; and I mean, she didn't give me any lectures. She did not have any books that she wrote. She did not have gold medals that she had won in her academic career. Nothing like that. And, yet she allowed me to witness and experience grace in its truest form in the way she accepted the disease. And, the way she accepted her death. It was as if she rejoiced in her death in that she met the challenges of life with all the passion that she could bring into those last few months. And, the noble way in which she passed through those last few months of her life became indelibly tattooed on my cerebrum forever. And, so much of what we shared, we shared a lot of poetry together, we shared--and, with other patients also. I mean, just reading fiction is so important because it allows one to poach on experience of others. It allows one to stand in the shoes of others. It allows one to see whole lives evolve and consequences of decisions that they made examined and reexamined. It teaches you to learn about yourself because you declare your feelings for one character and not for another. You like this one, you hate this one, and this gives you insights into yourself. So, for me, learning to deal with real human tragedies has been tremendously helped by the great writers of our literature. |
| 1:01:23 | Russ Roberts: I was listening to you talk about J.C., who you write about beautifully in the book as well, and you talk about that she had no tangible accomplishments like a book. No tangible signifiers like a gold medal. But when I think about her and people like her and people we know like that is that she is an artist. Her raw material was the tragedy of her disease, and she someone molded and crafted it into something extraordinary. And, I think that's the privilege a doctor can have, a nurse can have. I was recently visiting my dad in the hospital and he was there for five days and not in very good shape at 89, and the nurses who I saw every day have this great gift. They have the gift to give and they have the gift to receive, and that gift of receiving is often forgotten. I asked one of them, 'This is such a hard job--why do you do it?' He just said, 'Well , it's rewarding.' He said more than that, but for him it was clearly a labor love, which is the highest level, I think, someone in a caring profession can bring to that. I have to quote Emory Austin. In your book you quote her saying, 'Some days there won't be a song in your heart. Sing anyway.' And, I think someone who is dying--and of course we're all dying to some extent--but someone who's dying in extremis. Someone who is dying in pain and loss of dignity and anguish, to sing anyway is the highest form of art, it seems to me. Azra Raza: Yes , absolutely. You're so right in saying the things you just said. For me, I'll tell you that one of my most favorite fiction books of all time is of course Moby Dick, by Melville. For one reason, it helped me understand the storms and the souls of men that make them go whaling. But, for another, at one point he says something to the effect, I don't remember the exact quote, but something to the effect that--Pequod was the whaling ship on which he was standing--and he said something like, 'The deck of Pequod was my Harvard and my Yale.' Which means that experience can teach you in an instant so much more about the mystery and the essential wonders of what makes us such complicated human beings and how each of us deals with the questions of mortality and questions of living and dying. I do think that the patients' corporeal language write books in instances for us if we have the eyes--not just the eyesight, but the insight to appreciate what they are telling us. |
| 1:04:50 | Russ Roberts: Talk about the role of listening as a doctor and why it's important. I think it's a lost art for all of us, but I think particularly for doctors who are filling out their electronic forms and racing to the next patient. I think the luxury of listening is frequently lost. We've had some doctors talk about it before here on the program, but I'd like to hear it from you. What role does it play in your practice? Azra Raza: I read about a study where, if you put a finger in front of your eyes and start moving it, let's say, to the right and keep staring straight in front, eventually the finger will move out of your peripheral vision and then it will disappear, right? At some point. But, not for the deaf. It doesn't disappear in the peripheral vision that quickly for the deaf. Which means that they are seeing more seeing-ly than us. And the same way I insist to the younger doctors who are in training with me that they have to hear more hearing-ly. It's not enough to just sit silently and let the patient talk. But, how do you hear more hearingly, is the question. Right now the doctor-patient relationship is such that 80% of our time is spent in front of computers and 20% is spent in face to face interactions; and when there are deep concerns that are torturing a patient, they can't express it immediately. An average of two minutes of conversation has to occur uninterrupted before the patient will start to express, even, what is keeping them up at night or what their real issues are. And, yet doctors are known to interrupt a patient every 18 seconds. So, I mean, everyone means well. It's not that we are heartless oncologists who are just trying to do everything for a paycheck and just finish the 12 patients we have to see in the morning and rush out and finish the paper--no, it's not that. Somehow, it's disorienting. It's very distressing. It's terrifying to have to look so deeply into the agony that is in front of us, and I do think that it has to be done, though. If we can't help our patients to live better lives, we don't have to let them have to be a wreck, emotional wrecks. We have to help them. And that comes from really taking a human interest, which means you have to bring all your emotional, spiritual, physical, intellectual abilities to bear, and learn how to concentrate and focus on what is the patient's real issue. Not just the cure part, but the healing part of it is as important. I hope that answers your question. Russ Roberts: In the aftermath of your loss of your husband, you write about the profusion of inappropriate things that people say in attempts of consolation. I think about this from time to time: I think people blunder badly. In Jewish practice, when you go to the home of a mourner, Jewish law says that you're not to speak until the mourner speaks. I think people find this very difficult and some of this makes us uncomfortable; and we tend to blurt out things that often are worse than being silent. You talk about that as an example in your own personal situation. What I've always thought about this, is--this is one of those rare examples where a black and white rule like that is actually quite helpful. Sometimes those rules are just the best we can do. But the idea to sit in silence with a person who's suffering and saying nothing--that silence is yelling at us often, 'Talk, talk, talk. Say something.' And, just to sit there and let the other person speak first. And, I've always thought of that injunction is about allowing the--is to keep you from saying something inappropriate. But I think it also has a deeper meaning, which is it's to get you to listen. It's not just 'Don't talk.' It's, 'Listen.' I like that rule. I think it's a really helpful rule to start, but I'm curious what advice you give people in situations of tragedy for how to behave and how you--you don't have to go into the ones that didn't help you, but I'd be curious if you would talk about some of the ones that did help. Azra Raza: I mean, there were some wildly absurd reactions from people. Like, somebody came after Harvey died and offered to take me out to singles bars. Another person wanted to console me in a way, but the manner in which he did it was quite outlandish. He said, 'Azra, I'm so sorry Harvey died. But, don't worry. You'll join him soon and you two can live happily after ever in heaven.' That was really breathtakingly strange to me. Russ Roberts: And, then there was that one of, 'He's gone but you look great.' Azra Raza: Oh yeah. That one. Russ Roberts: 'Congratulations. Don't be sad. You look fabulous.' I think there's a terrible challenge in our culture these days that no one's allowed to be unhappy. Mourning is against the rules. So, if you look sad I've got to try to cheer you up. I can't ever just let you be sad. I've got to find something. 'Your food's delicious. Your house looks great. Lovely outfit.' Azra Raza: But, it's actually the inability of people to communicate with each other. I mean, especially emotionally. So, what you see around you are people who are unable, in fact, not just to communicate with each other but then to give sympathy and to receive sympathy, also. In a way it reminds me very much of the "Sounds of Silence," by Simon and Garfunkel, because basically that is the meaning of, what is the sound of silence? Is it the rustling of leaves, the sound of silence? Is it the flowing water in a brook when you're sitting in a forest and listening to the sounds of silence? What is the sound of silence between two individuals? Especially when one is a caregiver and the other is a patient. Very important to be able to take advantage of this kind of syntax. I think that some of the best times I--I'm very lucky, actually, Russ, because the disease that I treat, myelodysplastic syndrome, as you know, is a pre-leukemic condition. So, patients live a long time often. And we have a very unique way of developing long-term relationships because I'm seeing them every week or every other week, and taking them through many, many physically demanding situations like severe, profound anemia compromising the quality of life deeply, and yet giving them blood transfusions, which suddenly reverts them back to an energetic self for a few days; and when I see them during those days they're so different than when their hemoglobin was six grams. And, taking them through this for sometimes 10 and 20 years, and meeting them regularly every two weeks is a very unique privilege. And in these interactions, there are many times when we are just listening to music, listening to things together. Or just silence, actually. But, being together, and then suddenly speaking up and communicating at a level which is so profoundly different. Russ Roberts: I think silence is underrated. One of the advantages of being the host of this program is I've become a better listener and I've forced myself to become silent. I was thinking about the episode I did recently with Ryan Holiday where we talked about Marina Abramovic, who sat in silence for days across from a stranger--a set of hundreds of strangers at the Museum of Modern Art for an exhibition a few years ago. A documentary was made of it; it's an extraordinary documentary. And, I think we have a tendency to think, 'Well, silence is nothing. Silence is wasted. Silence is when nothing happens.' And, yet for me, increasingly as I get older and get better at silence--I'm not great at it but I get a little better--they're the deepest times. The most unforgettable times are often just being present for someone. And, that must be a big part of your daily life as a cancer doctor. Azra Raza: Yeah. Absolutely. I mean, I think many people who are devastated by silence and cannot tolerate it have to be distracted by all sorts of devices or general things in life[?]. I find that once they learn how to appreciate it, silence is responsiveness. We can listen to things behind the clamor of the world. |
| 1:16:32 | Russ Roberts: I want to try something a little bit strange at the end of this conversation, before we do, I want to let you close and let you talk about if you much optimism. And you've seen a lot of suffering and a lot of joy, and you write about it in this book in a beautiful way. There's some despair at the state of things, which I think listeners have heard in our conversation. Are you optimistic about the future? Do you think there's hope for a better approach to these challenges? Azra Raza: I almost feel like Leibniz: That, the world is the best of all possible worlds. Because I do feel very optimistic. Russ Roberts: I think that's Voltaire. I think that's Volatire in Candide. Is it also Leibniz? Does he say that, too? Azra Raza: Voltaire wrote Candide as a parody of Leibniz. He made fun of Leibniz. Russ Roberts: Okay. I didn't know it was Leibniz he was poking fun at. Okay. Azra Raza: Absolutely. Dr. Pangloss is, in Candide, that's who Leibniz is supposed to be. Because Dr. Pangloss is forever declaring in Candide that, 'Oh it's the best of all possible worlds. The nose is there because the spectacles have to rest on it. It's the best of all possible worlds.' Yeah. But, at the risk of sounding like Leibniz, I do think that the technology is so superb right now, Russ. I mean I could not have imagined 20 years ago that I would be living in a world, when I go back to Karachi and I'm caught in a traffic jam-- and when you're caught in a traffic jam in Karachi at the red light, often the homeless people and beggars will start knocking at your door. This started happening to me recently when in Karachi a beggar started knocking on the door, and before I could bring the window down, his cell phone rang. And, he answered cell phone and looked very concerned. So, when he got off the phone, I said, 'Is everything okay?' Now I got worried about him. And, he said, 'No, no. Everything is fine. That was my wife on the cell phone telling me that there's a bigger traffic jam near the university.' She's telling me to take an Uber to get there. So, technology has such power to transform our entire daily lives. I mean, when you commented earlier that it's a very difficult, insurmountable-almost, problem, I beg to differ with you on that now, because I think that the paradigm can shift overnight like it did from a typewriter to a word processor. From having a telephone booth to make calls, to even homeless beggars in the most impoverished countries in the world having access to computers they are carrying in their hands with powers that were unimaginable just 30 years ago. So, all I'm saying is, instead of going after the last cancer cell all the time--yes, we should continue doing that for our current patients--but at the same, let's turn to the first cell. Let's set the new goal. Let's incentivize this goal financially and let the race begin. And, then what we have seen can happen is that the human genome required collaboration and competition simultaneously between hundreds of thousands of investigators, but then what 20 years ago took 15 years to do to sequence the first genome and cost over a billion dollars, today can be done in a few weeks for the cost of a few hundred dollars. This is where technology can transform everything within a decade, is what I am saying. And, at the rate technology is moving, it will be faster and faster going ahead. I'm very optimistic for the future of cancer. |
| 1:20:57 | Russ Roberts: I want to close, I said try something a little bit different. I want to close with a--I'm actually going to sing something, which is a little out of character. I don't know if I've ever sung--I've probably sang something on this program before. But, there's a paradox in your book which is, as I've made it clear I think, there's a lot of despair and sadness in the book, and yet there's an immense amount of joy and you've really--all the patients, many of them who've passed away, the ones who passed away are immortal because they're in your book. Their song is out there. And, it's really an incredible thing. One of the things that your book forced me to think about is the preciousness of life and how, somehow, how is it possible that we have this great gift? We know it's finite. We don't like to think about that it's finite; but we know. It's our great tragedy and our great knowledge, our great insight. We go through life knowing it won't last forever, and we think about it often as if it does, which allows us to get annoyed at traffic jams and home repairs that don't work and all of the petty disagreements we have with the people we love. And, it's strange that we can go through life that way if we're not careful. Well, we all go through it to some extent that way. So, when I was thinking about that and reacting emotionally to your book, I was struck by a song by Susan Werner. It's called "May I Suggest," and we'll put a link up to it. It's a beautiful, live version that she does. But, this is the way it ends. Which your book inspired me to think about more intensely even than I usually do. It goes like this: This is a song
Comes from the west to you.
Comes from the west, comes from the slowly setting sun.
This is a song
With a request of you,
To see how very short the endless days will run.
And, when they're gone
And when the dark descends,
Oh we'd give anything for one more hour of light.
And, I suggest this is the best part of your life. So, this is the best part of her life. Azra Raza: Oh. How beautiful, Russ. Russ Roberts: So, this is the best part. This is me talking to you and whoever is listening. And, it's hard to remember that and your book reminds me to remember it. So, thank you so much. Azra Raza: Thank you, Russ. It's been absolutely a wonderful experience talking to you and thank you for all you do. I love your podcast, by the way. Russ Roberts: My guest today has been Azra Raza. Her book is The First Cell. Azra, thanks for being part of EconTalk. |
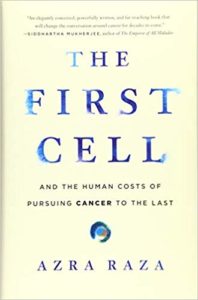 Author and oncologist Azra Raza talks about her book The First Cell with EconTalk host Russ Roberts. Raza argues that we have made little progress in fighting cancer over the last 50 years. The tools available to oncologists haven't changed much--the bulk of the progress that has been made has been through earlier and earlier detection rather than more effective or compassionate treatment options. Raza wants to see a different approach from the current strategy of marginal improvements on narrowly defined problems at the cellular level. Instead, she suggests an alternative approach that might better take account of the complexity of human beings and the way that cancer morphs and spreads differently across people and even within individuals. The conversation includes the challenges of dealing with dying patients, the importance of listening, and the bittersweet nature of our mortality.
Author and oncologist Azra Raza talks about her book The First Cell with EconTalk host Russ Roberts. Raza argues that we have made little progress in fighting cancer over the last 50 years. The tools available to oncologists haven't changed much--the bulk of the progress that has been made has been through earlier and earlier detection rather than more effective or compassionate treatment options. Raza wants to see a different approach from the current strategy of marginal improvements on narrowly defined problems at the cellular level. Instead, she suggests an alternative approach that might better take account of the complexity of human beings and the way that cancer morphs and spreads differently across people and even within individuals. The conversation includes the challenges of dealing with dying patients, the importance of listening, and the bittersweet nature of our mortality.

READER COMMENTS
Eric
Mar 23 2020 at 11:15am
About the necessary failure of reductionism…
Reductionism must fail because both the Taj Mahal and biology are examples of “specified complexity” in which the function comes from the specific arrangement of the parts, which cannot be discerned by studying any of the parts individually.
An arrangement of specified complexity is
not Arbitrary as the complexity in granite is arbitrary. You can’t throw bricks together in a random pile to get the Taj Mahal.
not Required by the laws of physics and chemistry as the structure of crystals is. Bricks do not inherently incline toward a Taj Mahal arrangement.
not Trivial. You don’t get a Taj Mahal by being accidentally lucky with a chance arrangement of bricks.
Exactly the same is true of biology. Origin of life researcher Leslie Orgel wrote that “In brief, living organisms are distinguished by their specified complexity.”
Reductionism must fail because you cannot derive the working functional arrangement from any study of the parts. The correctly working arrangement isn’t in the bricks or in the nature of the bricks. It cannot be inferred or understood from the bricks.
The obstacles of moving past a reductionist approach certainly do include this type of inertia, but that is not the greatest obstacle.
The hardest obstacle is the fact that in every case where we can trace significant specified complexity back to its cause, the cause always invariably includes the influence of minds and intentionality. Even for an emergent appearance of specified complexity (e.g. language or economic systems), the arrangement always involves a distributed collaboration of designing minds acting intentionally.
The idea that life is the result of mind, design, and intentionality is regarded as intolerable. So we persist in a futile and doomed reductionist attempt to try to discover how mindless bricks will unintentionally build themselves up into a Taj Mahal, despite the reproducible scientific reality that mindless bricks are invariably content to remain piles of rubble.
Ethan
Mar 24 2020 at 1:55pm
Eric,
I don’t have much to add to your above statement. I just want to reach out and compliment you on your thought provoking comments here and elsewhere.
I am just guessing that you are the same Eric in other episode’s comment sections, but I really enjoy the insights you share when you choose to do so. I loved the discussion you sparked in the Peter Singer episode as well as the John Gray episode. Based on those comments (as well as some push from an episode of the “Emergent Order” podcast), I read “Abolition of Man” and found it so fascinating. I never knew much about C.S. Lewis previously ,but I found his insight on the Tao and the refutation of the possibility of principles outside of it incredibly thought provoking as well as accessible.
I also love the formulation above in regards to complexity. I have been looking to learn more in regards to complexity as a discipline after learning of Taleb’s work. If you have any recommendations on how to dive into the “art”ful nature of irreducibly I would love to hear them.
Anyway, thank you again for your engagement in these comments. I look forward to more of them in the future.
Cheers!
Eric
Apr 1 2020 at 12:08pm
Thank you for your kind encouragement.
Life depends on information for building, regulating, and coordinating a dynamic dance of numerous molecular machines. Cancer can be different from person to person and from cell to cell because there are many different ways to impair or disrupt these information systems, some resulting in the “brake failure” of unrestrained rapid cell division.
You asked for “art”ful nature resources. The persistent failure of reductionist thinking and the need for a new biological paradigm is seen most vividly in the context of the origin of life.
Anything by Stephen Meyer is excellent and his first book is a great examination of the issue of the origin of life and of the specified complexity life requires.
The Mystery of Life’s Origin was the ground breaking 1984 textbook that exposed the fatal problem of reductionist explanations for the specified complexity of life. Now a new updated edition with new added chapters has just been released.
Please see also the resources in my reply below to Scott.
Eric
Apr 8 2020 at 9:57am
P.S. Regarding your request, here is a free extended excerpt from an update to The Mystery of Life’s Origin that discusses the pivotal significance of the discovery that life depends on specified complexity, which is different from mere order. Cancer derives from various corruptions of that specified complexity.
Scott
Mar 26 2020 at 11:04pm
Eric – I like your insight “The hardest obstacle is the fact that in every case where we can trace significant specified complexity back to its cause, the cause always invariably includes the influence of minds and intentionality.”
I will ponder this more deeply.
One initial question – Do you see this as a ‘gatekeeper’ issue?
The domains I am more focused on seem to yield insights from complexity, data science, and design thinking. I think many scientists would be happy to learn new tools if they help move the ball forward on their domain.
Science-minded people may view the world through a reductionist/deterministic lense, and may find dissonance with the root of intentionality. But that is a non-obvious insight… Perhaps after working successfully with these tools, their world views may be more accepting of such a precept?
The main issue called out in the podcast is around training and the status quo view. I would note, there are groups evangelizing the underlying concepts of complexity and emergence in digestible ways for people of all backgrounds, such as the Santa Fe Institute. They offer online classes, and a very active social media group called Complexity Explorers that looks at a variety of topics through a complexity science lense and has high-quality discussions.
Thanks for the great comments!
Eric
Apr 1 2020 at 12:09pm
Thank you for your encouragement. Thomas Kuhn distinguished between incremental changes that are easily welcomed and revolutionary paradigm shifts, which are more prone to be resisted and can be quite difficult. The old paradigm believed that life could be understood in a reductionistic way as the result of chance and necessity (laws) acting mindlessly on matter, but life’s pervasive dependence on specified complexity requires a major paradigm shift.
Corrupted genetic information can lead to cancer. Yet even if we knew everything that could be known about the physics and chemistry of the parts of an information medium, that would still never explain the functional information stored there. Understanding ink and paper cannot explain a written recipe.
The articles and books of Phillip Johnson were pivotal to exposing the prevailing philosophical commitment to materialism in science, which imposes the doomed obligation of presuming a mindless reductionist foundation.
Cancer is a failure within the systems sustaining life (e.g. the brakes on cell division). There is growing acceptance of the need to understand life in terms of Systems Biology, life as interacting systems. David Snoke has written about the fruitfulness of systems engineering concepts within systems biology. Reviewed here and here.
The Evolutionary Informatics Lab is also doing revealing foundational research and writing regarding complex specified information.
Please see also my reply above to Ethan.
krishnan chittur
Mar 23 2020 at 6:44pm
This was a beautiful episode – glad to be introduced to people like the good doctor who refuses to accept our progress in cancer treatment and want us to do better. I was also struck by what I heard (but not surprised) – we still do not know how a drug combination used for decades actually works. The tissue bank in combination with patient phenotype (properties, disease states etc) could be extraordinarily valuable in the hands of a machine learning/AI expert/company if (big IF) we can connect the information in the tissues studied using today’s methods with mechanisms. Far too often AI/ML provides astonishing insights but do not provide good actionable information unless the computer work is coupled to targeted, specific experiments in the laboratory (in vitro or in vivo). The good news is that as we collect more tissue samples and characterize them with any/all of the methods we do have (imaging, sequencing, high throughput screening) we will accumulate actionable insights not just for cancer, but for other diseases. Thanks for the gift of the episode.
John Wolfe
Mar 23 2020 at 6:55pm
Greetings, two things. Some time ago I may have commented on therapeutic drugs with something like ‘we should refrain from calling them life-saving as most are symptomatic treatment and do not resolve the underlying disease’. In any case, in today’s episode that seems to have been pointed out in the part that speaks to many drugs being altered in a minor way, enough to qualify for a new patent. I am not discounting the value of drugs. It seems to me that frequently using the ‘life-saving’ comment is promoted by the industry and is not often the case.
Second, my 65-year-old brother was diagnosed with MDS quickly followed with AML diagnosis two years ago. He became a patient of the University of Wisconson hospital where he went through much chemo leading up to a bone marrow transplant which failed. Good news is that about three months later he received a stem cell transplant. March 1 was his one year anniversary and he has been in fine health, good labs, etc. from about 3 months after the stem cell transplant.
I guess there is one more good news in his case and that is he had an ACA policy with no lifetime limits so he had very comprehensive coverage.
JonB
Mar 24 2020 at 12:14am
So sorry, we are not that wealthy as a society.
I can get next gen arbitrary tissue metabolomics and genetic sequencing for about $2000 total cash price for a patient with an unknown disease but then what?
If patient finds out they have 34,000 DNA variants of unknown significance and 20 metabolites with z-scores greater than 2, how does this change management?
Multivariate analysis is very very hard to translate into clinical practice. It all start with reductionism….in other words what is the known meaning of the individual data point. One rapidly discovers in this business that most of this data you find has minimal scientific investigations into its function. Commonly there are 2-3 labs in the world that know just a tiny tiny bit about a particular gene or protein or metabolite. Most of the others are amateurs….Society hasn’t been wealthy enough to support the reductionistic foundation to do this sort of work until very recently….
Once you have identified 200# likely candidates, then what? Machine learning is phrenology. Full stop. It tells you nothing about underlying physiology or pathophysiology. Waste of money but looks good on a grant….
A standard lab like GeneDX has 200 MD and PhDs attempting to understand the raw data of 3 billion base pairs. The wealth required is not the technology of DNA sequence acquisition but the intellect driving the data compression. This is just the first layer, Subsequently, you need another layer to translate their best guess on likely genetic variation into known physiology and pathophysiology. Then you need another layer to develop pharmaceuticals with adequate efficacy and safety
Our society is not yet wealthy enough to do this well for every disease…cancer, diabetes, vascular disease, depression…ad infinitum.
There is nothing to be angry about here. These are hard hard problems. Institutions likely the FDA and NIH are deeply corrupted with public choice problems. Everyone know this….but there is a lot of wreck in the economy and still other areas of the economy progress rapidly. Why not medicine?
Would think a little bit more as a practicing oncologist about what are the institutional barriers which slow the bace of innovation….obnoxious IRBs, clinical liability concerns, peer pressure to not stick out, state medical boards, etc. The public would be outraged if they knew how much effort it takes to satisfy every bureaucrats rice bowl. The COVID 19 test fiasco is no surprise to anyone in the business.
Good luck with your Biobank
Jerry
Mar 24 2020 at 10:26pm
JonB
Completely agree with you! She seems to be arguing that there is a solution by data mining a tissue bank. Not sure how screening a tissue bank for mutations is going to lead to new therapies in MDS. Also not sure how finding early mutations in bone marrow of asymptomatic patients is going to change the trajectory of their disease. Screening patients for a disease where you have no treatment just leads to stage migration rather than an actual impact on the natural history.
Stephen Clively
Mar 24 2020 at 6:09am
Ain’t that a kick in the guts. Here we are not far into the worst year of the 21st century so far and EconTalk has knocked another one out of the park.
I tried reading the comments already posted on this site but after listening to the end of the podcast I just couldn’t concentrate on them.
Although I’m going to have to think about my reaction to this episode for some time, I think Russ should sing again when he thinks the timing is right. That is, when he thinks it’s the right time to make a good portion of his audience melt down.
Marilyne Tolle
Mar 24 2020 at 3:16pm
I listened to this excellent podcast with a knot in my stomach. I lost my husband to a rare form of appendix cancer almost two years ago. His cancer was detected too late – as a stage 4 – five years earlier, through a combination of negligence, incompetence and bad luck.
A year later, it was my father’s turn to be diagnosed with cancer too late – stage-4 lung cancer in his case. Unlike my husband, he had been asymptomatic. My father’s treatment was stopped three weeks ago and he is now in palliative care. Because of the travel ban, I will not be able to be with him when he goes.
In my darkest hours following my husband’s passing, I looked into assisted suicide in Switzerland, in case I too were diagnosed with stage-4 cancer at some point. Listening to Dr Raza’s take on the current state of cancer detection and treatment, which I’m all too familiar with, hasn’t dissuaded me from taking that option seriously.
Marilyne Tolle
Mar 24 2020 at 9:26pm
“In Jewish practice, when you go to the home of a mourner, Jewish law says that you’re not to speak until the mourner speaks. (…) And, I’ve always thought of that injunction is about allowing the–is to keep you from saying something inappropriate. But I think it also has a deeper meaning, which is it’s to get you to listen.”
Beautifully said.
It includes listening to the silence of the mourner’s ineffable sadness, and simply being.
It reminds me of Parker Palmer’s recounting of how a friend would visit him during his severe depression and massage his feet in silence.
This is what Palmer said about it:
“And it became, for me, a metaphor of the kind of community we need to extend to people who are suffering in this way, which is a community that is neither invasive of the mystery nor evasive of the suffering but is willing to hold people in a space, a sacred space of relationship, where somehow this person who is on the dark side of the moon can get a little confidence that they can come around to the other side.”
Scott
Mar 26 2020 at 11:19pm
Very similar concepts extolled by Ram Dass. He spent a lot of life working with the dying.
Here is a low fidelity summary – the idea is to be with the dying and their pain. They will feel your presence and love, that you are with them sharing their experience. When they are ready they will relinquish the pain and there will be only truth, and a calm passage to the next life. Being with them in that process is a gift to you too.
Jerry
Mar 24 2020 at 10:22pm
Dr. Raza has clearly thought deeply about the barriers to improving the lives of her current and future patients. However, in her complaints against reductionistic thinking she has actually become reductionistic. I would argue that the premise that cancer is one disease permeates a great deal of her arguments. However neoplastic diseases represent a wide variety of ailments that have vastly different pathopysiologies and natural histories. Also, her focus on MDS has biased her view of the advances in many other tumors. In addition, there have been legion examples of single targets of treatment that have produced significant cures. For example, targeting the protein product of the 9,22 translocation in CML with the drug imatinib produces cures in 80% of patients. Prior to this treatment CML was universally fatal with and average survival of 5 years. Another example of a targeted treatment that has produced cures is Herceptin in breast cancer. This drug’s use in breast cancer after surgery has dramatically reduced cancer deaths for these women. The latest frontier is immunotherapy (not CAR-T as discussed in the episode) such as Keytruda. In a recent study of a combination of immunotherapies in metastatic melanoma (a disease that just a few years ago was universally fatal and most patients lived less than a year) now has over half of patients living longer than 5 years and likely 30-40% cured of their disease. These medicines and many others are not simply making a few months improvement but rather adding many years of life and curing patients. As a practicing oncologist for 20 years I have seen these remarkable advances, which have limited side effects compared to chemotherapy, improve dramatically the lives of my patients. These advances have happened because of the “reductionistic” principles that Dr. Raza is so against. I hope that your listeners do not think that cancer care has not advanced in the last 30 years because in fact when looked at outside of Dr. Raza’s speciality of MDS there have been unbelievable advances. I personally use very little chemotherapy (poison) and am now using a majority of targeted therapies and immunotherapies.
Now the issue of price is a different issue, but this is clearly not limited to pharmaceuticals but rather is most dramatically seen in the “non-profit” hospital setting’s use of 340-B pricing and DRG exemption.
Fasih Zulfiqar
Mar 25 2020 at 10:59pm
I think this might be my favorite Econtalk episode–or any podcast episode for that matter. I, too, am from Karachi and resonated with miss Azra, especially the beggar anecdote. Alas, the importance of poetry in modern Pakistani families has declined–a lot. I myself don’t know many ghazals, but I love the ones I do know; there’s just something profound about them.
I admire the work that you do miss Azra. Pakistan needs more people like you–the entire world does. Thank you for this brilliant episode, and for the heartfelt song at the end, Russ.
Patrick Allen
Mar 30 2020 at 5:46pm
The discussion on “slash/poison/burn” reminds me of a scene in “Star Trek IV: The Voyage Home.” Some of the crew, including Dr. McCoy, is transported back to current San Francisco (which in this case was 1986). While walking through a hospital Dr. McCoy is appalled by the barbaric treatment of cancer patients: i.e., chemotherapy.
Jim
Mar 31 2020 at 1:42am
Really fantastic discussion.
When Paul Allen, co-founder of Microsoft, was diagnosed with Hodgkin’s Lymphoma in 1982, he was treated with radiation, according to Wikipedia.
Today, chemotherapy seems to be the go-to treatment, which is a significant step down in toxicity from radiation. “Slash, poison, burn” may still be with us, but the treatment has become more nuanced as doctors do a better job optimizing the formula, dosage and testing.
I’m not a doctor, but I don’t think it’s accurate to say that cancer treatment has stood still with gains only coming from early detection and lower smoking rates. The gradual optimization of the decades old formula has likely materially saved and improved the quality of lives.
Why haven’t we advanced beyond “slash, poison, burn” is a good question, but it’s not like there hasn’t been any progress as portrayed in the discussion.
Paul G Kamp
Mar 31 2020 at 6:04pm
What a beautiful episode.
I am sure the doctor is aware of the research. My sense is that due to people like her we may be on the verge of transitioning from the “Slash/Poison/Burn” into something new.
Something gained from the broad insight we all gain from the free flow of information. Tempered by the emotional element that this episode speaks to so beautifully.
I remain hopeful that things will improve. I’d like to cite two items:
How these impossibly tiny organs could finally end animal testing
New blood test can detect 50 types of cancer
I hope these and many other things help change how cancer is treated so we can spend more time together.
Mark Maguire
Apr 4 2020 at 12:40pm
A documentary was mentioned in this podcast, BREAKTHROUGH, so I watched it. Wonderful to see it. I wanted to find out more about Dr. Raza’s comment: “But, nowhere do investigators point out that these T-Cells also cannot differentiate between a normal cell and a cancer cell….. So, what they actually do is kill the whole organ”. I had never heard that, but it seems like a show-stopper. I’m not a medical person, and I have not studied this subject.
The documentary featured the case of a melanoma patient who has been cancer free since being treated with James Allison’s immune system therapy. Nothing is mentioned about destruction of an organ. So I’d like to explore that a bit more.
Chase Eyster
Apr 5 2020 at 3:35pm
Dr. Roberts,
Thank you for your deeply moving discussion with Dr. Raza. Powerful, insightful, thought-provoking podcasting at its best. I am grateful to have the opportunity to listen to your conversations with the innovators and visionaries you invite to EconTalk. Stay well!
Brendan
Apr 9 2020 at 5:16pm
I’ve enjoyed listening to Econtalk for many years, but I’ve never been as profoundly moved as I was listening to this episode. I felt tremendously privileged to get the opportunity to listen to these two amazing minds discussing such an incredibly important topic.
Bravo Russ! Thank you for the gift of this wonderful conversation.
Comments are closed.